In the researched medical ward the average number of patients per registered nurse was high, and only a third of the overall nursing hours were conducted by nurses with a bachelor's degree. Although, the number of staff did not deviate from that expected in European hospitals , the observed staffing levels could provoke rushed judgments about low quality of care. However, it should be noted that in the observed hospital the management calculates the number of registered nurses and nursing technicians together , ignoring evidence on higher nurse staffing levels being reflected in better patient outcomes .
With the use of two profiles of nursing staff, the productivity levels, number of nurse working hours and nurse–patient ratios appear to be good. But this hospital is employing cheaper nursing technicians instead of registered nurses, and this low-cost approach ignores actual patients care needs, actual unit occupancy rates, and staff competences and, as a consequence, the graduate staff are overloaded. The shift to value-based care is just one of many fundamental changes happening in healthcare today.
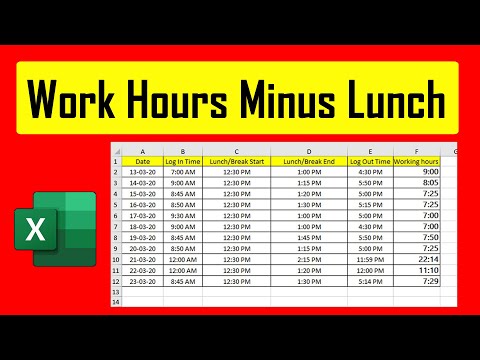
Healthcare organizations across the continuum are challenged to increase productivity AND reduce costs while maintaining proper staff levels to meet patient needs and compliance requirements. Hours per patient day is a common industry expression used to trend the total number of direct nursing care hours , compared to the number of patients as the HPPD ratio. Using a the "nursing hours per patient day" is a way to monitor and improve quality of care and service. And in many states, hospitals, clinics, acute care facilities, long-term care and senior living facilities must report the HPPD data to the Department of Public Health.
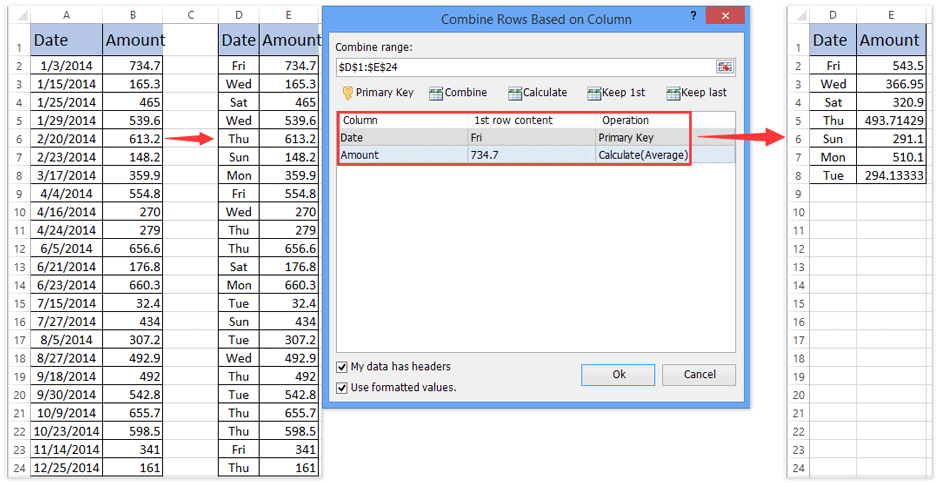
OSHPD's Hospital Disclosure Report measures employment in terms of productive hours for each of RNs, LPNs, unlicensed aides/orderlies, management and supervision, administrative and clerical, and other labor categories. Most hospitals use their payroll system, not their actual unit-level staffing grid, to complete the survey, and thus the data are subject to errors that might exist in any payroll system. For example, hospitals might not consistently measure hours worked by nurses normally assigned to one unit but "floated" to another. The number of patient days or services provided in each revenue unit is reported, enabling calculation of hours per patient day, hours per patient discharge, and/or hours per service provided. Unit types can be aggregated or examined separately (e.g., HPPD for medical–surgical acute care only). Correlations between the AHA and OSHPD datasets for inpatient days and RN employment were high overall, at least 0.9.
The means of RN and LPN employment were not statistically significantly different, while computed hours per patient day were statistically different in the OSHPD and AHA datasets. Most hospitals provide the staffing data to OSHPD and AHA from payroll systems, which might contain several types of measurement error. First, these systems do not delineate direct patient care from nondirect care in productive staff or hours, and thus overestimate the amount of direct nursing care received by each patient.
For example, a nurse might change the unit to which s/he is assigned, without a change in pay, and this change may not be reflected in the payroll data in a timely fashion. The panel reviewed current staffing ratios of registered nurses, licensed practical nurses, and nursing assistants, and concluded the current levels are inadequate. Seventeen out of the 30 conference participants endorsed a final staffing recommendation that established 4.55 total nursing hours per resident day as a minimum threshold. Noting that nursing management and leadership are central to providing a high quality of care in nursing facilities, the panel also recommended the director of nursing in nursing facilities have a minimum of a bachelor's degree.
Many researchers and health care leaders want to measure nurse staffing according to the workload of each nurse, although "workload" does not have an agreed-upon definition. Most hospitals can easily report the average number of productive nursing hours per patient day ("hours per patient day" or HPPD), because they keep data on nursing hours and patient days. Based on an analysis of 1999 cost report filings, all of Connecticut's nursing facilities licensed as CCNHs exceed the minimum nursing-staff-to-resident-day ratios established under the regulations.
Although the regulations require 694 annual minimum nursing staff hours for CCNHs, all nursing homes licensed under the CCNH category had 754 annual hours or more per bed in direct care staffing. Based upon the data contained in the cost reports, there was an average of 1,435 direct care hours per resident per year; more than double that required under the regulations. We used a hierarchical four-grade nursing care classification system to assess nursing care levels for patients at different acuity levels. This system identifies the staffing levels required to achieve appropriate nursing care, although unfortunately it is not used in practice yet.
When we compared the actual nursing levels, the conventional patient-to-nurse ratio and the nurses needed on the basis of patients' classification, we found severe shortages. Individual patient requirements were not respected, as a 38% shortage of registered nurses was measured. Therefore, nursing staff requirements should be considered as a predictor of the quality of nursing services , and having enough nurses to meet patient needs could be reflected in higher patient satisfaction with nursing care .
This study showed also that patients were more satisfied when the proportion of baccalaureate nurses in the nursing workforce was higher. While these results support the findings of previous studies , there is limited evidence correlating hospital nurse staffing with patient satisfaction in the literature . Research reports positive patient outcomes when staffing levels allow a maximum of six patients to one registered nurse on a medical ward . Similarly, other research finds that more patients per nurse result in higher rate of care left undone . The survey requested that hospitals provide data for a representative medical–surgical unit in the hospital. Survey questions focused on nursing hours worked on that unit, discharges and patient days on the unit, nurse-to-patient ratios, number of vacancies, and average time to recruit a RN to the unit.
Both hours per patient day and the nurse-to-patient ratio were reported directly by unit managers, enabling a direct comparison of these methods of measuring nurse staffing. The program review committee compared the minimum regulatory nursing staff requirements to actual hours of nursing staff reported by facilities in its Medicaid cost reports. There are several caveats attached to the data used for an analysis of the distribution of nursing staff among Connecticut's nursing facilities. First, the number of hours reported for RNs, LPNs, and nurse aides by facilities is self-reported and not audited by DSS. In addition, there are no uniform definitions for reporting on nursing staff hours.
Thus, while some facilities may report paid hours, which include any vacation, sick, and personal time accrued, others might report actual hours worked. Third, nursing staff hours are reported on an annualized basis, but daily, weekly, and monthly nursing staff fluctuations may vary considerably. Finally, data were available for only 226 facilities out of the 253 licensed CCNHs, and estimates are based on an average 95 percent occupancy rate, rather than a facility's actual occupancy.
Table 2 summarizes the critical care and medical–surgical nurse staffing and patient days data reported by CalNOC and OSHPD. OSHPD reports a greater number of RN and LPN hours as well as patient days, and all differences are statistically significant. The greater number of nursing hours reported by OSHPD is consistent with OSHPD's productive hours including non-direct-patient-care hours, which may include RNs in special roles such as clinical specialists or infection control managers. The correlations between RN hours, LPN hours, and patient days are relatively high, ranging from 0.73 to 0.92.
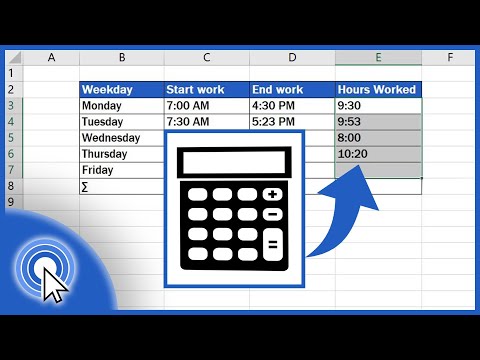
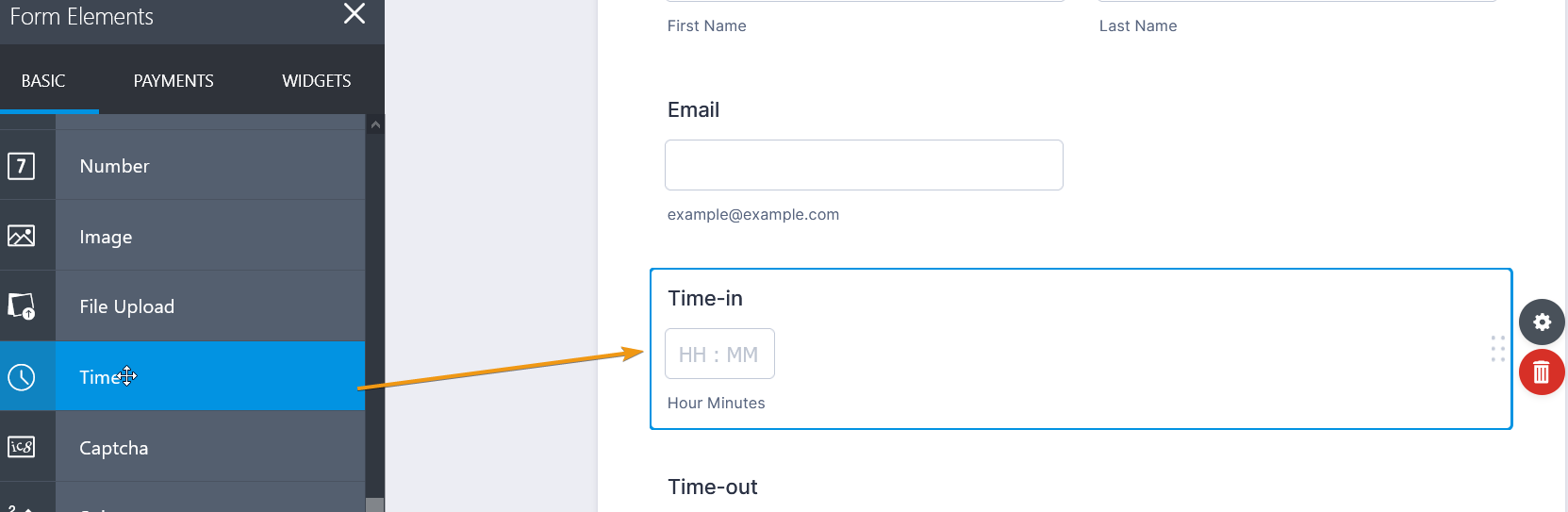
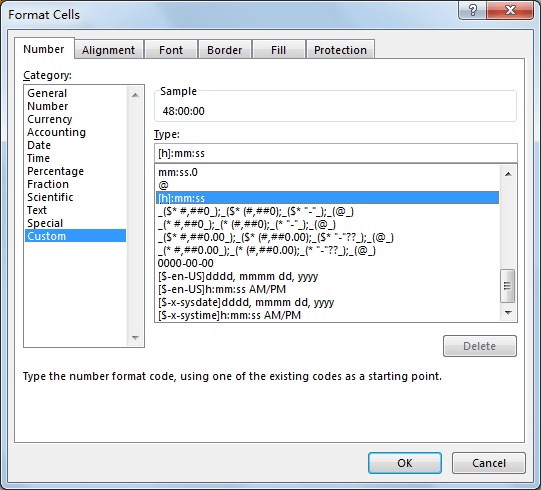
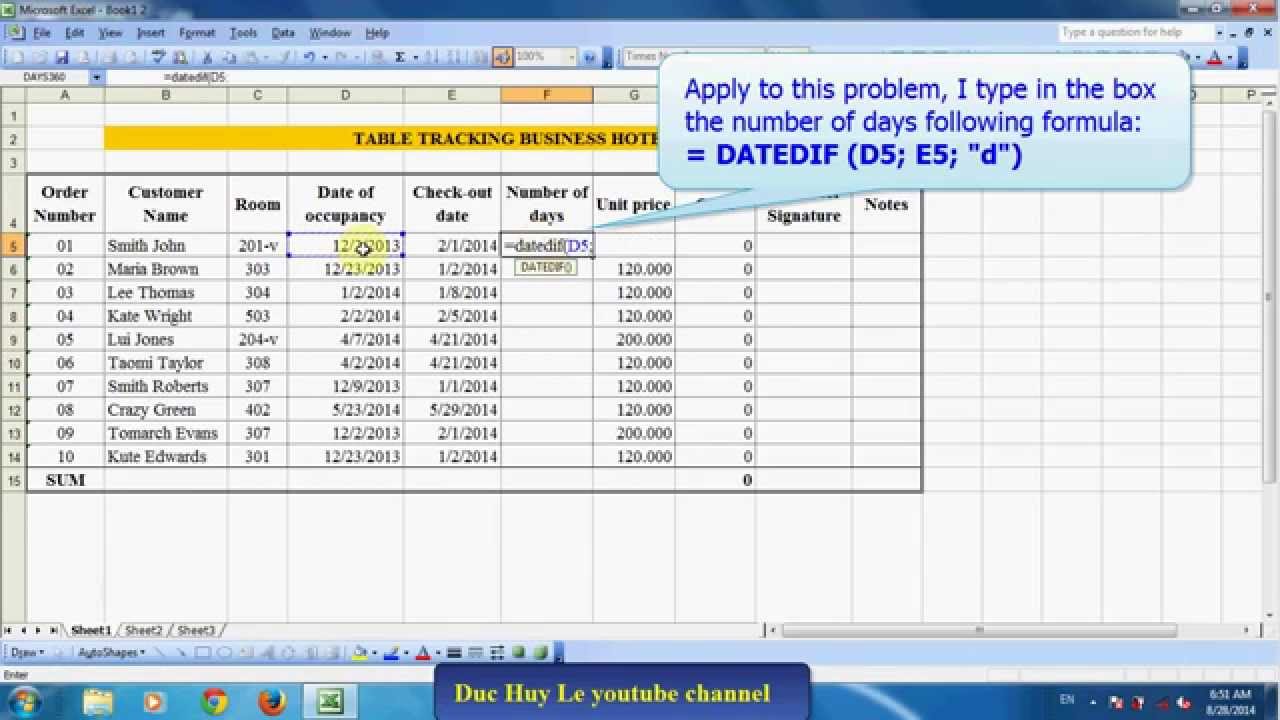
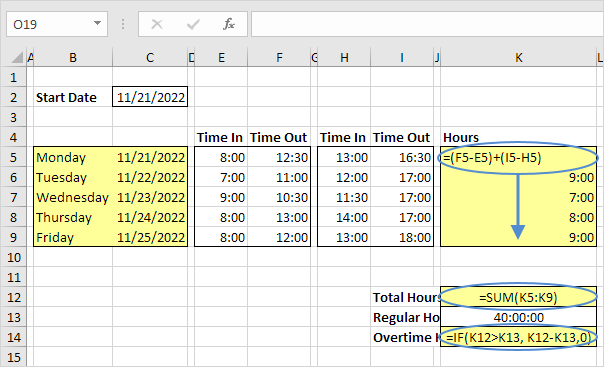
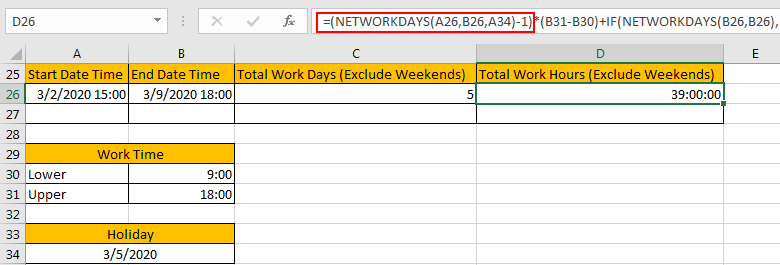
The correlations are higher for critical care than for medical–surgical care. Currently, the Nursing Care Hours per Patient Day formula is the unit of analysis that determines staffing requirements in hospitals. It is a calculable formula that is used as a method of staffing and for budgeting nursing hours . Nursing Care Hours per Patient Day are calculated by multiplying the number of staff delivering direct nursing care by the hours worked during the shift and then dividing that number into the average daily census at a specific designated time.
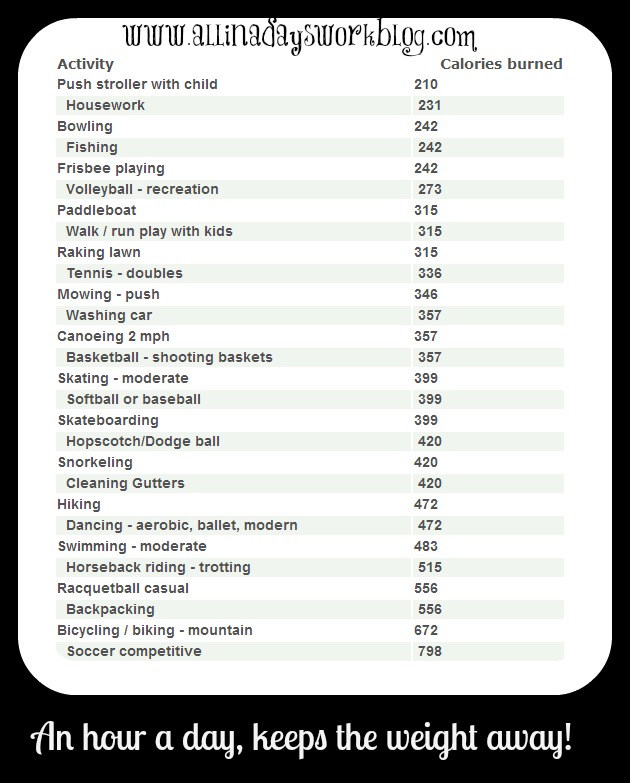
For the purposes of this study, the midnight census was chosen as the designated time. Nursing Care Hours per Patient Day were studied and the data from both Quarters under review were analyzed and compared. The current minimum total nursing staff hours per resident in a CCNH bed is 694 hours annually. This means each resident can expect to receive 13.31 hours of direct care each week. Figure III-1 shows the minimum number of nurse and nurse aide hours required per- resident-day is 1.9 hours - an average of less than five minutes of care per resident, per hour.
In terms of licensed nursing personnel for a CCNH, the minimum requirement is .64 hours per day. If nurse aides provide all of the non-licensed care that is allowed, they will provide a total of one hour and 16 minutes of care per resident each day. Table III-I describes the minimum nurse and nurse aide staffing requirements for CCNH and RHNS beds in Connecticut. The regulations establish minimum standards for nursing-staff-to-resident ratios during two segments of a 24-hour day and are expressed in terms of staff hours per patient . For example, on average the regulations require each resident receives 84 minutes of total nurse and nurse aide care during the 7 a.m. Observations suggest that registered nurses need to engage in a great variety of tasks, and spend a great deal of time locating the information needed for individual patients.
Calculator Hours Worked Per Day Health education, clinical references, consulting, and coaching were the least frequent activities in the registered nurses' working days. We were not able to observe a fifth of the registered nurses' activities, as these were done outside the medical ward. These activities could thus not be classified in the observations, but were described by the staff as nursing tasks on other medical units, meetings with management, quality teams, and so on. Moreover, the results show that the patients noticed the individual attention they received from registered nurses while they cared for them, and that their explanations helped them feel more at ease. Nurses are known to spend more time with patients than other health professionals, and that enables them to show the caring attitude which is sensitive to patients' reports of quality of nursing care .
Registered nurses have a wide range of nursing knowledge and good communication skills, are alert to changes in the patients' status and have the competencies needed to do all the activities that arise in nursing care. Nursing technicians have fewer competencies, and care for fewer patients than registered nurses – certain tastes are thus not delegated from registered nurses to technicians, but the vice versa. This could mean that patients would benefit if mixed staffing models, like the one observed in this study, would include more nurses with bachelor's degrees. In fact, according to published studies hospital nurses spend from 7.3% to 54.2% of their time on direct patient care, from 0% to 59% on indirect care, and from 14% to 17% on personal time . Patient satisfaction is influenced by factors identified at the patient level along with nurses' kindness and competence with regard to performing technical procedures .
When items in the instrument represent patients' perceptions, there are no criteria against which criterion-related validity could be tested . Some researchers have argued that hours per patient day is the most precise measure of the amount of nursing care provided to patients (Budreau et al. 1999). However, hours per patient day do not accurately measure the impact of admissions, discharges, and transfers on the workload of nurses. Unruh and Fottler have demonstrated that nurse staffing measures that do not adjust for patient turnover underestimate nursing workload and overstate RN staffing levels.
While prospective unit-level databases such as CalNOC often include measures of admissions, discharges, and transfers, administrative databases do not include such measures. The program review committee believes the minimum nursing staff ratio suggested in HCFA's study is based on the most comprehensive and defensible research to date. Furthermore, the establishment of minimum nursing staff standards does not negate the federal and state requirements that nursing facilities provide adequate nursing staff to meet residents' needs. Minimum staffing thresholds merely establish a floor below which a facility cannot drop.
An analysis from the Journal of Emergency Nursing found that a calculation of hours per patient visit was the most frequently used method for determining staffing in the ED. This method requires dividing the number of actual paid hours by the total number of ED visits to calculate the number of staff hours per year. The authors pointed out that this type of system fails to take a few critical factors into consideration, including patient acuity, length of stay, and nursing workload. The authors discussed a tool that may be more accurate for calculating annual needs.
It incorporates key variables of patient volume, patient acuity, nursing interventions and activities, skill mix, and ED length of stay to determine the direct needs in an emergency department. There is also a chart in the article that can show how to use the tool to facilitate the calculation of the number of full-time equivalent nurses needed. The authors say that the tool can be used to determine staffing needs in the ED as well as for monitoring staffing indicators. Inpatient care unit does not include any hospital-based clinic, long-term care facility, or outpatient hospital department. "Staffing hours per patient day" means the number of full-time equivalent nonmanagerial care staff who will ordinarily be assigned to provide direct patient care divided by the expected average number of patients upon which such assignments are based.
"Patient acuity tool" means a system for measuring an individual patient's need for nursing care. Decisions about the adequacy and appropriateness of nurse staffing have long been based on functionally outdated industrial models that focus on work sampling and time-and-motion studies conducted in semi-simulated settings. Even today, the common method of staffing nursing units or identifying the staffing mix in hospitals is by identifying budgeted Nursing Care Hours per Patient Day. A traditional measure of nursing productivity, "nursing hours per patient day has never been satisfactory because 'patient day' as a measure of nursing output takes neither patient acuity nor quality of nursing care into accou nt". .
The 3.5 DHPPD staffing requirement, of which 2.4 hours per patient day must be performed by CNAs, is a minimum requirement for SNFs. SNFs shall employ and schedule additional staff and anticipate individual patient needs for the activities of each shift, to ensure patients receive nursing care based on their needs. The staffing requirement does not ensure that any given patient receives 3.5 or 2.4 DHPPD; it is the total number of actual direct care service hours performed by direct caregivers per patient day divided by the average patient census. Metrics such as hours per patient day and nursing hours per patient day , referred to by Carter as CHPPD, have been used for decades in the US to examine nursing productivity both within and between hospitals.
They are also used to determine staffing levels based on national or regional benchmarks and establish budgets for nursing departments. NHPPD usually refer to qualified nurses in the US, so may include only RNs with degrees or both RNs and those with older diplomas and/or licensed practical nurses. NHPPD are also used in several states in Australia and are usually used to describe qualified nurses only. This is why it is important to understand which staff are included before accepting staffing data.
The CalNOC data are less widely dispersed than the OSHPD data for the matched set of hospitals, suggesting that the CalNOC data might contain less measurement error. Nursing hours were on average higher in the OSHPD data than in CalNOC, likely because OSHPD data include nurse staff time spent on activities other than patient care. As a result, the distribution of nurse staffing per patient day is different between these datasets, with the CalNOC data producing somewhat lower hours per patient day than the OSHPD data. The correlations between estimates of hours per patient day are low, at 0.22 for total nursing hours and 0.32 for RN hours.
Moreover, undivided attentionand explanationwere positively correlated only with the volume of registered nurses' work hours. However, the item things are done without askingwas negatively correlated with the working hours of nursing technicians. The total in this equation provides the nursing hours per patient day, which helps nursing facilities understand what ratio of nurses to patients is best for them. For all licensed facilities nationwide, the average total nursing staff hours per patient day was 4.0 for January 2011 through February 2012, according to the Kaiser Family Foundation,.
When possible, hospital units or types of units were matched within each hospital. Productive nursing hours and direct patient care hours were converted to full-time equivalent employment and to nurse-to-patient ratios to compare nurse staffing as measured by different surveys. It is critical that clinical staff have access to HPPD levels and how they are calculated in a particular institution in order to inform their practice. Evidence-based care must use data and research on measures of productivity, patient satisfaction, quality, and financial accountability.
In the meantime, some hospitals are implementing a number of strategies to account for the staffing level on all units and to address bottlenecks in processing patient admissions, transfers, and discharges. At the heart of these activities is a shared desire to provide the best person-centered, timely, efficient, and effective care. As a nurse leader, you are expected to know what your average daily census is for your department and staff. Flexing your staffing levels to the volume that you have is key to your department being productive.
You may be asking yourself, where does patient safety and quality care come into consideration, instead of just dollars? There are also several evidence-based leadership studies that prove the higher the RN ratio to patient, the lower the adverse outcomes for the patients. The successful nurse leader learns to find the right balance between quality, safety, staff satisfaction, and fiscal responsibility in providing the most effective staffing plan. A relationship between staffing and quality of care in nursing homes is inherently logical. However, the correlation is difficult to demonstrate because of the complexities in defining and measuring quality, the lack of valid nursing staff data, and the differences in residents' acuity levels among facilities. The purpose of the analysis was to determine if facilities that received a high number of deficiencies reported less staff per resident day than those with zero or only one deficiency.